Acromegaly
Angeliki's story
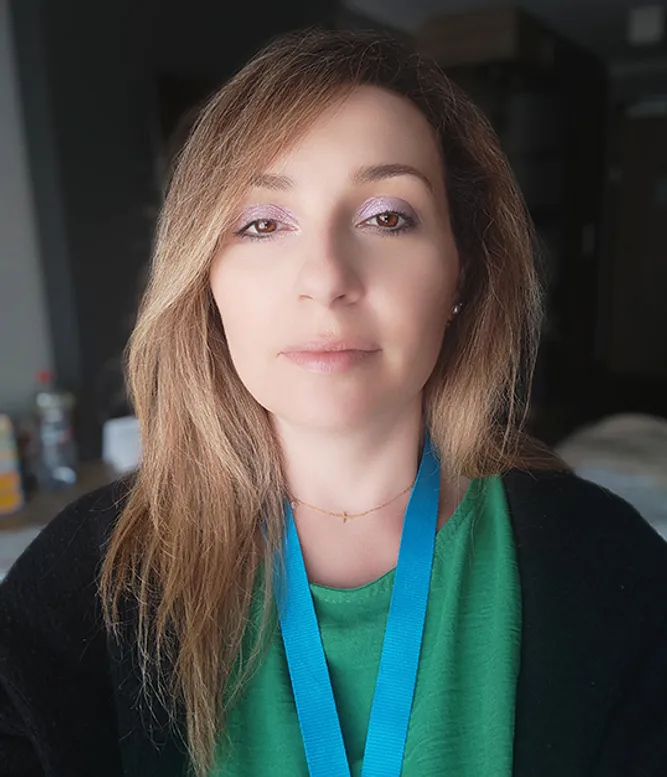
Angeliki felt like a bad wife and mother. But after being diagnosed with acromegaly, she realized how badly the disease symptoms had impacted her life.
Living with a serious disease
Angeliki was tired all the time, balancing her career in finance and life with a husband and two young children. “My family suffered the most, as I put all my energy into going to work and doing a good job. So, by the time I got home, I was exhausted and just slept,” she explains. “It wasn’t fair on my family – they could see I wasn’t well, but I blamed everything and everyone else. I felt like a bad wife and mother.”
For almost two years, Angeliki sought help from different doctors and specialists, but no one knew what was wrong. Over time, her vision became blurry, she experienced excessive night sweats, her mind was foggy so that she couldn’t concentrate, and she suffered with severe headaches. She stopped driving. Eventually, she was in so much pain, she couldn’t brush her teeth or even hold a spoon to feed herself.
“I looked in the mirror and didn’t recognize myself. Psychologically, as well as physically, it was a very bad time.”
When just 36 years old, Angeliki was rushed to hospital with a stroke. The surgeon discovered a tumor on her pituitary gland, which was affecting Angeliki’s growth hormone levels. She was diagnosed with acromegaly. “I felt so alone and didn’t know what was going on, or what was going to happen to me. The surgeon told me he wanted to treat this aggressively; he wanted to attempt to remove the tumor completely as I was so young.” By this stage Angeliki had lost her vision and the doctors didn’t know if she would get her sight back. She agreed to the operation.
Four days after being admitted to hospital, Angeliki underwent surgery. The tumor was completely removed. When Angeliki came round from the anesthetic and opened her eyes she could see – and for the first time in years was no longer in such incredible pain. “The relief was instantaneous. I couldn’t believe it; it was miraculous!”
However, trauma to the pituitary gland during surgery has left her with adrenaline deficiency which comes with its own symptoms and problems. Still, Angeliki does not regret having the tumor removed.
“I am not the same person I was before I had acromegaly – I am different and there are some things I still cannot do. I hoped to have another baby, but this wasn’t to be. But I have found a quality of life that for me, personally, is good.”
The importance of patient communities
As Angeliki had so little time between diagnosis and surgery, she was unable to seek support from patient groups before her operation, but once she was home from hospital, she started to find out about acromegaly. “At first I thought I was the only person in Greece who had this disease!” she laughs. “I found an amazing patient organization in the UK who were so kind and made me feel not alone.”
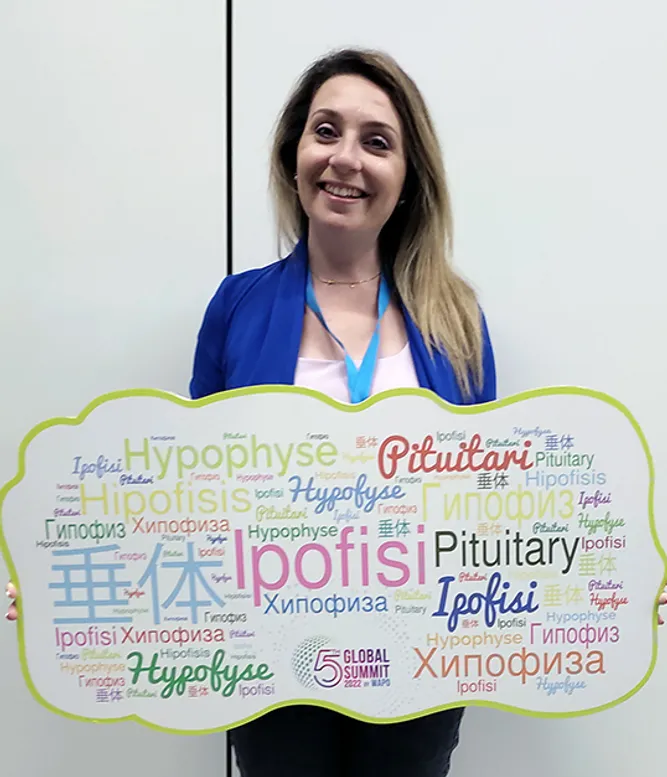
Angeliki has since organized a small group of patients in Greece, which tries to communicate and educate about this disease and share experiences with other patients. She was also a Board Member of the World Alliance of Pituitary Organizations (WAPO) until recently. “I am passionate about raising awareness and understanding about this disease,” Angeliki explains. “If a person who has recently been diagnosed with acromegaly is reading this, I want to tell them not to be afraid. Yes, this is a chronic disease – but there is life after diagnosis.”
Symptoms
- Enlarged hands and feet
- Altered facial features
- Joint problems
- Muscle weakness and fatigue
- Anxiety and depression
- Headaches
- Soft tissue swelling
- Excessive sweating
- Sleep apnea
- Visual disturbances
Diagnosis
Diagnosis is usually made by an endocrinologist, often a pituitary specialist (neuroendocrinologist), although referral may be made by doctors from a range of medical specialties. In patients with symptoms of acromegaly, diagnosis includes the measurement of growth hormone levels and magnetic resonance imaging (MRI) to detect a tumor in the pituitary gland.
Treatment
Surgery and/or medical treatment, sometimes in combination with radiotherapy.
Explore more
Learn more about acromegaly.