Agromegaly
Crys' story
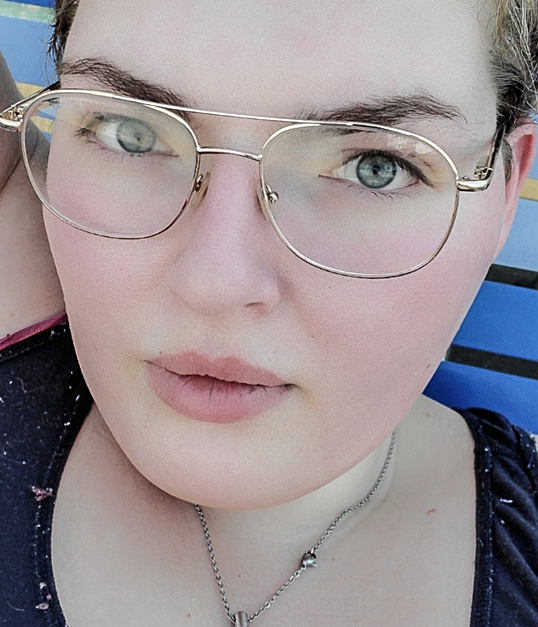
Six years ago, after years of severe headaches and passing out in the shower, Crys was diagnosed with a pituitary tumor. She was only 20 years old.
Getting used to another quality of life
“I definitely panicked. Especially as a kid or young adult, when someone says: ‘hey, you have a brain tumor’, what is your reaction supposed to be to something like that? I saw my life flashing before my eyes. In the midst of this whirlwind of doctors, I had tunnel vision from panicking, and I thought the tumor was called acromegaly. I did not realize that it was a whole disease, that it was going to be a lifelong thing. I thought I was just going to have the tumor removed and everything would be fine,” explains Crys.
The closer she got to the surgery, the more she stressed, mostly due to the worry about being under anesthesia for a longer period.
“So I was doing a bunch of research and that was when I realized that acromegaly is a chronic illness. I had to process the diagnosis in my own time before I could take in any information.”
Crys had been suffering with blurry vision and headaches for years without realizing the cause. At the age of 17, she started having severe migraines. Crys’ ophthalmologist found a swelling on her optic nerve, but it wasn’t until she was rushed to hospital after passing out in the shower that Crys was diagnosed with a pituitary tumor – and acromegaly.
“I was always big, but my dad is very tall, and his side of the family are all very large, so we thought that I just took after him. But once I was given that diagnosis the doctor asked me to show her pictures of myself from five years ago.
"...After looking at the pictures, I could see how acromegaly had affected me and it made a lot of sense. I definitely have the whole being large thing going on,” explains Crys.
Crys used to work within retail, working within shoe sales. But after the surgery she was no longer able to manage the fast-paced environment. Today she works night shifts at a hotel: “Working is very difficult. The jobs I had prior to the surgery were a lot more physically demanding. Now basically I have to do the laundry at night, and that is about it.”
“Some days are better than others, in how I view what the future looks like for me and my family. I have depression, because the quality of life that I was used to has been taken away and I have to think, ‘Am I going to be able to do this in ten years?’ It is hard for me to stand up for long periods; I do not have the endurance I had before. I need to modify what I do – I can’t clean my house in 20 minutes or cook an elaborate meal. I use mobility aids to help me get around,” Crys explains.

Raising awareness
Crys is grateful that she was diagnosed so young and is keen to raise awareness of her condition: “Awareness is a big thing and I do my best to talk about it with everybody that seems interested, because I do not think it is as much a rare disease as it is a disease not talked about. So you’ve got people who are walking around with symptoms, but they have no idea. I was lucky getting diagnosed as early as I did. Most people do not get diagnosed until they are middle aged.”
But the COVID-19 pandemic has unexpectedly opened possibilities for Crys’ future: “Eventually, I want to be a teacher and the pandemic has actually made it easier because now you can do more online. Whereas I was expecting to be on disability in five years, I now might be able to work full time from home. Maybe the world is becoming a little bit more accessible, and that is really nice to notice.”
Symptoms
- Enlarged hands and feet
- Altered facial features
- Joint problems
- Muscle weakness and fatigue
- Anxiety and depression
- Headaches
- Soft tissue swelling
- Excessive sweating
- Sleep apnea
- Visual disturbances
Diagnosis
Diagnosis is usually made by an endocrinologist, often a pituitary specialist (neuroendocrinologist), although referral may be made by doctors from a range of medical specialties. In patients with symptoms of acromegaly, diagnosis includes the measurement of growth hormone levels and magnetic resonance imaging (MRI) to detect a tumor in the pituitary gland.
Management
Surgery and/or medical treatment, sometimes in combination with radiotherapy.
Explore more
Learn more about acromegaly.